Anti-depressants work by balancing chemicals in your brain called neurotransmitters that affect mood and emotions. These depression medicines can help improve your mood, help you sleep better, and increase your appetite and concentration. Here are more details of some types and how they work in the body and brain.
1: Selective Serotonin Reuptake Inhibitors (SSRIs)
2: Serotonin and Noradrenalin Reuptake Inhibitors (SNRIs)
3: Tricyclic and tricyclic-related drugs
4: Monoamine Oxidase Inhibitors (MAOIs)
First, here is a note from the Royal College of Psychiatrists:
“Are the newer ones better than the older ones?
Yes and no. The older tablets (Tricyclics) are just as effective as the newer ones (SSRIs) but, on the whole, the newer ones have fewer side-effects. A major advantage for the newer tablets is that they are not so dangerous if someone takes an overdose.”
Let’s start with number 1, the SSRI’s (newer ones) which in my research were most commonly detailed –
The Mayo Clinic . org (USA) states on their website that:
“SSRIs, a commonly prescribed type of antidepressant, can help you overcome depression. They can ease symptoms of moderate to severe depression, are relatively safe and typically cause fewer side effects than other types of antidepressants do.
Serotonin is one of the chemical messengers (neurotransmitters) that carry signals between brain cells.
SSRIs block the reabsorption (reuptake) of serotonin in the brain, making more serotonin available. SSRIs are called selective because they seem to primarily affect serotonin, not other neurotransmitters.
SSRIs also may be used to treat conditions other than depression, such as anxiety disorders.
The Food and Drug Administration (FDA) has approved the following SSRIs to treat depression:
Citalopram (Celexa)
Escitalopram (Lexapro)
Fluoxetine (Prozac)
Paroxetine (Paxil, Pexeva)
Sertraline (Zoloft)
Vilazodone (Viibryd)
Fluvoxamine, an SSRI that’s approved by the FDA to treat obsessive-compulsive disorder, is also sometimes used to treat depression.
All SSRIs work in a similar way and generally can cause similar side effects, though some people may not experience any. Many side effects may go away after the first few weeks of treatment, while others may lead you and your doctor to try a different drug. If you can’t tolerate one SSRI, you may be able to tolerate a different one, as SSRIs differ in chemical makeup.
They say that taking your medication with food may reduce the risk of nausea. Also, as long as your medication doesn’t keep you from sleeping, which can also be a side effect, you can reduce the impact of nausea by taking it at bedtime. Other side effects can be drowsiness, dry mouth, dizziness, headache, blurred vision, diarrhoea, nervousness, agitation or restlessness, also possible sexual problems.”
According to Anxieties.com – the most effective SSRIs for anxiety are:
Fluoxetine (Prozac), Sertraline (Zoloft), Paroxetine (Paxil), Fluvoxamine (Luvox), (Escitalopram oxalate) Lexapro. And Citalopram (Celexa).
They say on their website that these newer types of antidepressant medications were introduced into the U.S. in the 1980’s, beginning with Prozac (fluoxetine). These drugs offer a different chemical structure than the cyclic antidepressants and therefore produce different effects on the brain. Primarily they assist the brain in maintaining enough supply of the neurotransmitter serotonin. For instance, researchers associate a deficiency of serotonin with depression and obsessive-compulsive disorder and implicate it in panic disorder and other psychological problems. These medications are called selective serotonin re-uptake inhibitors, abbreviated to SSRIs.
They explain that SSRIs can be helpful for depression, panic disorder, social anxiety, obsessive compulsive disorder, generalized anxiety and PTSD. They are well tolerated medications that are safe for medically ill or frail patients and safe in overdose. There are no withdrawal effects unless the patient stops them abruptly, and no dependency develops. They generally do not promote weight gain.
But they also state that there are possible disadvantages:
“It takes four to six weeks to notice significant therapeutic benefits from the SSRIs. The full range of benefits can take twelve weeks. Patients often experience a temporary worsening of anxiety symptoms during the first two weeks of treatment.
Abrupt discontinuation of the SSRIs could cause flu-like symptoms.
And all the SSRIs can be expensive.
Plus they tend to cause sexual problems more than other Antidepressants or Benzodiazepines. In fact, they say, this may be their main limitation, occurring in as many as 35 to 40% of patients. (It is unclear whether these problems are evident in one SSRI more than others.)
Other possible side effects (apart from initial agitation and sexual problems) can be Nausea, insomnia, or headaches. Some can also cause dry mouth, diarrhoea, constipation, loss of appetite, stomach pain, dizziness, drowsiness, fatigue, yawning, increased sweating, or muscle/joint pain.
Some should not be taken during breast feeding or when trying to conceive.”
(They had a lot more detail on the specific drugs listed, but I think that is too much to include here, although their site can obviously be referred to if readers should wish to know more.)
The NHS in the UK states that SSRIs are mainly prescribed to treat depression, particularly persistent or severe cases, and are often used in combination with a talking therapy such as cognitive behavioural therapy (CBT).
They say that SSRIs are usually the first choice medication for depression because they generally have fewer side effects than most other types of antidepressant, and that SSRIs can be used to treat a number of other mental health conditions, including generalised anxiety disorder (GAD), obsessive compulsive disorder (OCD), panic disorder, severe phobias, such as agoraphobia and social phobia, bulimia, and post-traumatic stress disorder (PTSD). They also say that SSRIs can sometimes be used to treat other conditions, such as premature ejaculation, premenstrual syndrome (PMS), fibromyalgia and irritable bowel syndrome (IBS), and that occasionally, they may also be prescribed to treat pain.
They explain the way that SSRIs work similarly to the USA sites already quoted from: “Serotonin is a neurotransmitter (a messenger chemical that carries signals between nerve cells in the brain). It’s thought to have a good influence on mood, emotion and sleep. After carrying a message, serotonin is usually reabsorbed by the nerve cells (known as “reuptake”). SSRIs work by blocking (“inhibiting”) reuptake, meaning more serotonin is available to pass further messages between nearby nerve cells. It would be too simplistic to say that depression and related mental health conditions are caused by low serotonin levels, but a rise in serotonin levels can improve symptoms and make people more responsive to other types of treatment, such as CBT.”
They also add that “SSRIs usually need to be taken for two to four weeks before the benefit is felt. You may experience mild side effects early on, but it’s important that you don’t stop taking the medication. These effects will usually wear off quickly. A course of treatment usually lasts for at least six months, although longer courses are sometimes recommended and some people with recurrent problems may be advised to take them indefinitely.”
They continue with some useful warnings “SSRIs also need to be used with caution if you have certain underlying health problems, including diabetes, epilepsy and kidney disease. Some SSRIs can react unpredictably with other medicines, including some over-the-counter painkillers and herbal remedies, such as St John’s wort. Always read the information leaflet that comes with your SSRI medication to check if there are any medicines you need to avoid.”
They list seven SSRIs prescribed in the UK:
- citalopram (Cipramil)
- dapoxetine (Priligy) – I note that this one was not listed on US sites, although there was also one listed on US sites which is not listed here.
- escitalopram (Cipralex)
- fluoxetine (Prozac or Oxactin)
- fluvoxamine (Faverin)
- paroxetine (Seroxat), different trade names than the US ones
- sertraline (Lustral), different trade names than the US ones
I note that all of these have different trade names than the US ones, apart from the trade name Prozac.
Medical Daily . com has similar information on SSRIs, but includes some extra details :
“Serotonin is a neurotransmitter associated with feeling of wellbeing and happiness. These chemicals are naturally produced in the brain, but might be produced in lower quantities in people with depression. SSRIs block (inhibit) serotonin from being reabsorbed (reuptake) back into the nerve cells they came from — nerves typically recycle these neurotransmitters. This leads to an increased concentration of serotonin in the synaptic cleft, the space between the two communicating cells. Scientists believe all this extra serotonin can then strengthen communication between the nerve cells, specifically the circuits associated with mood regulation. And with higher connectivity, patients with depression can find relief from the hopelessness, extreme sadness, and lack of interest in life that they’ve become acquainted with.
Supported by the fact antidepressants often take a couple of weeks to begin working, some research has shown that rather than just improving connectivity, antidepressants work to grow and improve branching between nerve cells in the hippocampus. In one study on mice, for example, researchers found that when neurogenesis was blocked, the antidepressants stopped working. When it wasn’t blocked, they showed 60 percent more dividing cells in the hippocampus. This translated to improvements in anxiety and depression, too, as they became more willing to venture for food in a brightly lit place.
If more research shows that SSRIs stimulate neuronal growth, depression treatment may one day involve drugs specifically made to stimulate nerve growth, leading to faster and better outcomes.
Medical Daily . com also contained information about SNRIs, NDRIs, SARIs, and everything else. The ones we are specifically looking at are :
2: Serotonin and Noradrenalin Reuptake Inhibitors (SNRIs)
3: Tricyclic and tricyclic-related drugs
4: Monoamine Oxidase Inhibitors (MAOIs)
But there are a few extras listed here, which I will leave in as a matter of interest, and to round things off, particularly as one is related to dopamine, mentioned under one of the others we do need to discuss here.
“Again, the science behind depression treatment is based on the idea that connectivity between neurons must be improved. Therefore, all other antidepressants work in different ways to increase neurotransmitter levels between neurons. Here’s how:
Serotonin and norepinephrine reuptake inhibitors (SNRIs) inhibit the re-uptake of both serotonin and norepinephrine, the latter of which is sometimes involved in a system in the brain associated with responding to environmental stimuli that grabs a person’s attention and motivates them to do something.
Norepinephrine and dopamine re-uptake inhibitors (NDRIs) again inhibit the re-uptake of neurotransmitters; this time dopamine and norepinephrine. Dopamine is another neurotransmitter commonly associated with feelings of happiness and well-being.
Serotonin antagonist and re-uptake inhibitors (SARIs) work on serotonin in two ways: they inhibit the re-uptake of the molecule and prevent them from binding to cell receptors, thus causing the molecules to accumulate in the synaptic clefts.
Tetracyclic and tricyclic antidepressants were some of the earliest forms of antidepressant drugs. They work by inhibiting a number of neurotransmitters, including serotonin, epinephrine, and norepinephrine, from re-uptake as well as binding to nerve cell receptors.
On the occasions that neurotransmitters aren’t reabsorbed into the nerve cells, they’re broken down. Monoamine oxidase inhibitors (MAOIs) work to inhibit the enzyme monoamine oxidase from breaking down serotonin, epinephrine, and dopamine.
Because many of these antidepressants can cause life-threatening side effects, it’s important to consult with your doctor before taking them.
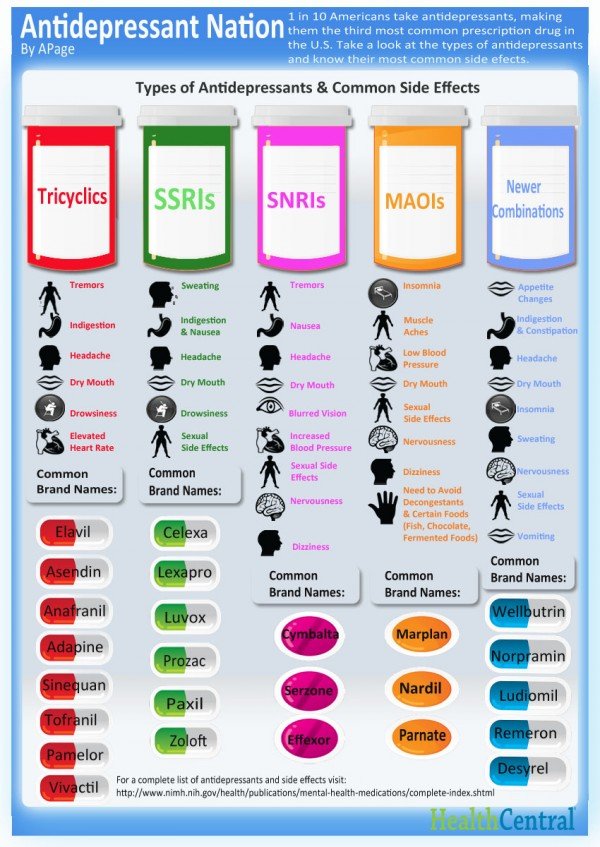
For more information on any of these drugs, see the table below from Health Central:
Other sites with information about our other 3 anti-depressant types :
2: Serotonin and Noradrenalin Re-uptake Inhibitors (SNRIs)
3: Tricyclic and tricyclic-related drugs
4: Monoamine Oxidase Inhibitors (MAOIs)
The .gov.uk website contains information about SNRI’s, including a lot of information about safety risks, which I really urge people considering taking them to read, but I will include the main information only here:
“Dual action serotonin and noradrenaline re-uptake inhibitors (SNRIs) are a class of antidepressant drug used to treat major depression and other disorders. They are a newer class of drug than selective serotonin re-uptake inhibitors (SSRIs), but act in a similar way, altering neurotransmitter levels in the brain, or prolonging their effects. SNRIs act particularly on serotonin and noradrenaline.
The SNRIs prescribed in the UK are:
- venlafaxine – brand names: Bonilux, Depefex, Foraven, Politid, Venlalic, Winfex, Efexor
- duloxetine – brand names: Cymbalta, Yentreve
Venlafaxine was the first SNRI to be marketed (in 1994) and is the most commonly used medicine in this class. It is used to prevent recurrence of major depressive episodes and to treat:
- major depressive disorders
- generalised anxiety disorder
- social anxiety disorder and panic disorder
For the treatment of major depressive disorder, generalised anxiety disorder and diabetic peripheral neuropathic pain, duloxetine is marketed as Cymbalta. For the treatment of stress urinary incontinence, duloxetine is marketed as Yentreve. Cymbalta and Yentreve should be prescribed for their correct intended use, and should not be used together.”
The Royal College of Psychiatrists say in an online leaflet that SNRIs have very similar side effects to the SSRIs, but that Venlafaxine should not be used if you have a serious heart problem. It can also increase blood pressure, so this may need to be monitored.
They say that Tricyclics work as well as SSRIs although they are older, but tend to have a few more possible side effects, and are more dangerous if someone takes an overdose.“Tricyclics commonly cause a dry mouth, a slight tremor, fast heartbeat, constipation, sleepiness, and weight gain. Particularly in older people, they may cause confusion, slowness in starting and stopping when passing water, faintness through low blood pressure, and falls. If you have heart trouble, it may be best not to take one of this group of antidepressants. Men may experience difficulty in getting or keeping an erection, or delayed ejaculation. Tricyclic antidepressants are dangerous in overdose.”
They also have information about Monoamine Oxidase Inhibitors (MAOIs):
“This type of antidepressant is rarely prescribed these days. MAOIs can give you a dangerously high blood pressure if you eat foods containing a substance called Tyramine. If you agree to take an MAOI antidepressant your doctor will give you a list of foods to avoid.
For a full list of side effects please visit emc.medicines.org.uk and type in the name of the medicine in the ‘Search for:’ section at the top of the page.”
They do give a lot more details about the in’s and out’s of taking anti-depressants if you want to look up more.
Mind.org.uk have this brilliant quote on the front of their website, which not only encourages people to use medication when needed, but gives a great example of they way it should ideally be used – for a brief period to enable you to find and use other ways to help you continue to recover.
“I took medication for six months. It helped lift the fog and gave me the energy I needed to tackle the root cause of my depression. There is no shame in taking medication to treat an illness.”
It also contains this information about SNRIs:
“The first of these was developed in the early 1990s, so they’re one of the newer types of antidepressant. They’re very similar in action to SSRIs, but they act on noradrenaline as well as serotonin. They have a more selective action than tricyclics, which means they’re better at targeting the brain chemicals which affect your mood, without causing unwanted side effects. They’re sometimes preferred for treating more severe depression and anxiety.”
Also this about Tricyclics:
“They’re the oldest type of antidepressant, first developed in the 1950s.
- They work by prolonging the action of noradrenaline and serotonin in the brain.
- They’re called ‘tricyclic’ because of their chemical structure, which has three rings.
- They tend to cause more unpleasant side effects compared with other types of antidepressants.”
And this about tricyclic-related drugs:
- They act in a very similar way to tricyclics, but they have a slightly different chemical structure.
- They tend to cause more unpleasant side effects compared with other types of antidepressants, but they’re less likely to cause antimuscarinic effects than tricyclics.”
From another part of the Mind site I got this explanation of the above –
“Antimuscarinic effects (sometimes called anticholinergic effects) is the medical term for a group of side effects which can occur with many different types of drugs – especially tricyclic antidepressants.
They include: blurred vision, confusion and agitation, constipation (which may become life-threatening if not treated), difficulty urinating, drowsiness, dry mouth (which can cause tooth decay in the long term), hallucinations, hot or dry skin, and decreased sweating, increased pressure in the eye, low blood pressure (taking hot baths increases this risk), rapid heartbeat and disturbed heart rhythm, and trembling.
These side effects can happen because, as well as affecting brain chemicals related to mood, the drug can also affect brain chemicals which control the different functions in your body.”
The Mind site also had this to say about Monoamine Oxidase Inhibitors (MAOIs):
“They work by making it harder for an enzyme (monoamine oxidase) that breaks down noradrenaline and serotonin to do its job, causing these chemicals to stay active in the body for longer.
- They can have dangerous interactions with some kinds of food, so when taking MAOIs, you need to follow a careful diet.
- Because of these interactions, you’re not likely to be prescribed an MAOI unless you’ve tried all other types of antidepressant and none of them have worked for you.
- They should only be prescribed by specialists.”
Wikipedia has more information about Monoamine Oxidase Inhibitors (MAOIs) which adds more positive information about them than I have quoted thus far:
“Monoamine oxidase inhibitors (MAOIs) are class of drugs that inhibit the activity of one or both monoamine oxidase enzymes: monoamine oxidase A (MAO-A) and monoamine oxidase B (MAO-B). They have a long history of use as medications prescribed for the treatment of depression. They are particularly effective in treating atypical depression. They are also used in the treatment of Parkinson’s disease and several other disorders.
Reversible inhibitors of monoamine oxidase A (RIMAs) are a subclass of MAOIs that selectively and reversibly inhibit the MAO-A enzyme. RIMAs are used clinically in the treatment of depression and dysthymia, though they have not gained widespread market share in the United States. Because of their reversibility and selectivity, RIMAs are safer than the older MAOIs like phenelzine and tranylcypromine.
Because of potentially lethal dietary and drug interactions, monoamine oxidase inhibitors have historically been reserved as a last line of treatment, used only when other classes of antidepressant drugs (for example selective serotonin reuptake inhibitors and tricyclic antidepressants) have failed.”
However Wikipedia adds that “New research into MAOIs indicates that much of the concern over their dangerous dietary side effects stems from misconceptions and misinformation, and that despite the proven effectiveness of this class of drugs, it is underutilized and misunderstood in the medical profession. New research also questions the validity of the perceived severity of dietary reactions, which has historically been based on outdated research.
However, this research also notes that many practitioners have a poor understanding of drug interactions, and “drug interactions can be serious, and concomitant medication use must be stringently overseen” as they “can cause a dangerous or fatal serotonin syndrome/toxicity”.
Wikipedia then goes on to say that “Newer MAOIs such as selegiline (typically used in the treatment of Parkinson’s disease) and the reversible MAOI moclobemide, provide a safer alternative and are now sometimes used as first-line therapy.”
And – “MAOIs have been found to be effective in the treatment of panic disorder with agoraphobia, social phobia, atypical depression, or mixed anxiety disorder and depression, bulimia, and post-traumatic stress disorder, as well as borderline personality disorder. MAOIs appear to be particularly effective in the management of bipolar depression according to a recent retrospective-analysis. There are reports of MAOI efficacy in obsessive-compulsive disorder (OCD), trichotillomania, dysmorphophobia, and avoidant personality disorder, but these reports are from uncontrolled case reports.
MAOIs can also be used in the treatment of Parkinson’s disease by targeting MAO-B in particular (therefore affecting dopaminergic neurons), as well as providing an alternative for migraine prophylaxis. Inhibition of both MAO-A and MAO-B is used in the treatment of clinical depression and anxiety.
MAOIs appear to be particularly indicated for outpatients with dysthymia complicated by panic disorder or hysteroid dysphoria, which involves repeated episodes of depressed mood in response to feeling rejected.”
Wikipedia does have a huge lot of extra information there if interested.
Other Possible Treatments

The Royal College of Psychiatrists has this very interesting section I would like to add to this article :
“What other treatments of depression are available?
It is not enough just to take the pills. It is important to find ways of making yourself feel better, so you are less likely to become depressed again. These can include finding someone you can talk to, keeping physically active, drinking less alcohol, eating well, using self-help techniques to help you relax and finding ways to solve the problems that have brought the depression on. For some tips on self-help, see our leaflet on depression.
Talking treatments
There are a number of helpful talking treatments for depression. Counselling is useful in mild depression. Problem solving techniques can help where the depression has been caused by difficulties in life. Cognitive Behavioural Therapy helps you to look at the way you think about yourself, the world and other people. For information about these and other forms of psychotherapy, see our leaflets on Psychotherapy and Cognitive Behavioural Therapy.
Herbal remedies
There is also a herbal remedy for depression called Hypericum. This is made from a herb, St Johns Wort, and is available without prescription. Because it is a herbal treatment, it is less well researched and there may be variations in the preparations on sale. Another problem is that it can interfere with other medicines like ‘the pill’. If you are taking other medication, you should discuss it with your doctor.
Light
You may find that you get depressed every winter but cheer up when the days become longer. This is called seasonal affective disorder (SAD). If so, you may find a light box helpful – this is a source of bright light which you have on for a certain time each day and which can make up for the lack of light in the winter.
How do antidepressants compare with these other treatments?
Over a period of a year, many talking treatments are as effective as antidepressants. However, antidepressants may work faster (see references). Some studies suggest that it is best to combine antidepressants and psychotherapy. Unfortunately there can be a waiting list for talking treatments in some parts of the country.
Hypericum, or St John’s Wort, seems to be as effective as antidepressants in milder depression, although there is little evidence that it works in more severe depressions.
Physical activity and self-help books based on Cognitive Behavioural Therapy can be effective treatments for depression.”
As a reminder though, I note that earlier in this article I also quoted the NHS as saying that St John’s Wort should not be taken alongside SSRIs –
“Some SSRIs can react unpredictably with other medicines, including some over-the-counter painkillers and herbal remedies, such as St John’s wort. Always read the information leaflet that comes with your SSRI medication to check if there are any medicines you need to avoid.”
My own previous research leads me to also add the following notes :

According to health and nutrition experts, including myself, good diet can play a huge part in preventing depression and other brain issues such as dementia.
Many nutrients are essential for good brain health.
Omega 3’s keep the lining of neurons healthy so that they don’t degenerate. Our brains need specific fats! Fish oil (DHA) is a good source, but if you are vegetarian you can make DHA from Flaxseed oil (linseed) as long as you have all the other nutrients and hormones needed to process it. Flax provides ALA – considered an essential nutrient because humans lack the n-3 desaturase enzyme required for its production. You can also get vegetarian DHA from algal oil.
Vitamin B’s are crucial for a good nervous system (more in a future article).
Vitamin D (sometimes called the sunshine vitamin) can help prevent the so called winter blues, and is also needed for the nervous system.
Many other nutrients are also crucial to brain function, such as zinc and iodine, and hormonal balance is important too.
Evening Primrose Oil can prevent migraines associated with periods for women, which do often affect mood, emotions, sleep, concentration, appetite, etc. and are related to hormonal changes.
It has also been shown that physical exercise is crucial to good brain health, partially due to it actually stimulating production of some feel-good brain chemicals. (It can even become slightly addictive due to this!)
Exercising the brain itself, by learning new things, has been shown to create new connections so that even if some parts of the brain malfunction due to amyloid plaque buildup (which destroys myelin), the new connections will ensure you do not suffer from alzheimer’s even if the older connections break down. You can see a video about this at – https://www.ted.com/talks/lisa_genova_what_you_can_do_to_prevent_alzheimer_s#t-821329
I would also speculate that mindfulness (or meditative visualisation, which I already teach people to use) could very possibly aid brain chemistry balance, as even just imagining your brain chemicals becoming balanced may very well cause them to be more so.
More about myelin and DHA from https://selfhacked.com/blog/myelin/
Myelin is an important part of the nervous system and is vital for optimal cognitive function. Myelin sheath is a cover (sheath) made out of fats and proteins that wraps around the axon (end) of a nerve cell. It insulates neurons so that they can send electric signals faster/more efficiently. Myelin is about 80% fats/cholesterol and about 20% proteins (dry mass). Oligodendrocytes and Schwann cells are types of cells that produce myelin. Schwann cells produce myelin in the body (outside the brain), while oligodendrocytes are found solely in the brain.
Oligodendrocytes are responsible for the formation of new myelin in both the injured and normal adult brains.
DHA (such as from fish oils) is essential for myelination. Animal models provide solid evidence that the consequences of dietary DHA deficiency are a high omega-6 to omega-3 ratio in brain fatty acid composition and deficiencies in learning and memory. Ref – https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4772061/#B142-nutrients-08-00099
“Docosahexaenoic acid (DHA) is the predominant omega-3 (n-3) polyunsaturated fatty acid (PUFA) found in the brain and can affect neurological function by modulating signal transduction pathways, neurotransmission, neurogenesis, myelination, membrane receptor function, synaptic plasticity, neuroinflammation, membrane integrity and membrane organization. The consumption of DHA leads to many positive physiological and behavioural effects, including those on cognition. Advanced cognitive function is uniquely human, and the optimal development and ageing of cognitive abilities has profound impacts on quality of life, productivity, and advancement of society in general. However, the modern diet typically lacks appreciable amounts of DHA. Therefore, in modern populations, maintaining optimal levels of DHA in the brain throughout the lifespan likely requires obtaining preformed DHA via dietary or supplemental sources.”
“Studies show that vitamin D3 induced a functional recovery and increased myelination in a rat model of facial nerve injury. The vitamin D receptor can increase the production of oligodendrocytes.”
Footnote:
I note that I haven’t been able to establish why preventing re-absorption would really be a good idea in the long run, as if nature intended for these chemicals to be re-absorbed rather than continually kicking around, surely there is a reason why it’s not ideal to have them constantly around. Is this perhaps what causes the side effects? Also I was beginning to wonder if people suffering some of those things listed as side effects, might actually have some issue with brain chemical imbalance causing them, or at least some other problem that might cause that imbalance? Also if we come off the drugs, is the body really able to reorganise to normal patterns? Is it just that while the drugs make us feel better we are able to find other sources of help such as CBT and Mindfulness (both of which I am currently studying), that then allow us to have more control over our own mental well-being, recognizing changes in the patterns and learning coping mechanisms? I think now, having read more, that this really is the case, the drugs are only meant to be used for a short while to enable other help or progress to be made, except I guess in some exceptional circumstances.
This whole area is very interesting but there is still so much we don’t know. Personally, as long as I was in a state to be able to seek alternative help, I would really rather not have to resort to using such drugs. There are a lot of people around who can help in other ways.
Julia Woodman



According to this nightmare article about part of the extremely dubious history of drug testing – https://jonrappoport.wordpress.com/2018/03/30/how-the-cia-hid-their-mkultra-mind-control-program/ – “SSRI antidepressants increase violent behaviour, including homicide.” and “Ritalin can induce hallucinations and paranoia.”
LikeLike
Tricyclic antidepressants like amitriptyline (Elavil), doxepin (Sinequan) and imipramine (Tofranil) can lower your body’s CoQ10 levels in your body so it may be helpful to take CoQ10 supplements, but please speak to your Doctor about this first to ensure it’s okay, for example doesn’t interfere with other meds, etc. Ref article by Dr Mercola – https://articles.mercola.com/vitamins-supplements/coq10.aspx which also discusses other forms such as ubiquinol for older people.
LikeLike